By Stefan Superina and Dr. Bob Bell
Fans watching the NBA Finals battle between the Toronto Raptors and Golden State Warriors may have noticed the Kaiser Permanente logo accompanying the media backdrop the Warriors use to conduct interviews with the press. A recently announced partnership between the American health services giant and the Golden State Warriors branded Kaiser as the team’s official physician, in addition to the role it already serves as the NBA’s official health care expert and consultant.
The Kaiser brand travels north of the border as well. During halftime of game two between the Raptors and Warriors, TV broadcasters Matt Devlin and Jack Armstrong announced a partnership between the Raptors and Kaiser Permanente to dedicate a newly created NBA Cares Learn & Play Centre at the Jimmie Simpson Recreation Centre in Toronto.
So, what exactly is Kaiser Permanente? Why is it able, unlike Canadian hospitals which seek philanthropic support, to act as a philanthropic donor and corporate sponsor?
For starters, Kaiser Permanente is the largest integrated non-profit healthcare system in the United States, generating $79.7B USD in operating revenues in 2018 alone with a “profit” of $2.5B USD. To put that into perspective, that’s far more than the entire Ontario healthcare system spends on delivering services ($61.3B CDN). Kaiser Permanente is one of many healthcare organizations in the US that pays big money to associate their brand with popular American sports teams in an effort to grow their customer base and capture market share in the burgeoning American health management economy.
In our continuing approach to healthcare system analyses, we are evaluating Kaiser Permanente because many astute observers have heralded its integrated system of care as a model that should be replicated in other jurisdictions around the world. And as Ontario embarks on its own journey of integrated care with the Ontario Health Team model, we wondered what could be gleaned from the Kaiser model to inform healthcare system improvement in Ontario.
Kaiser Permanente: Then and Now
Predating Medicare in Canada, Kaiser’s roots can be traced back to the 1930s when Dr. Sidney Garfield opened up the Contractor’s General Hospital for construction workers employed building an aqueduct in the Mohave Desert. Instead of workers coming to see Dr. Garfield only when their injuries became more serious (due in part to the financial barriers of obtaining fee-for-service care ), Dr. Garfield theorized that a system of preventive medicine financed through pre-payment (workers would be charged 10 cents a day for prepaid care) would allow workers to seek treatment earlier, as well as offer opportunities for health education and healthy lifestyle modification.
In 1941 prominent shipbuilder Henry Kaiser invited Dr. Garfield to devise a similar model of care for workers in his shipyard. Kaiser Permanente formally opened its first hospital at the Richmond Shipyard in 1942 to provide emergency care to acutely ill and injured workers. The hospital included six aid stations and later a larger hospital in Oakland to care for the most critically ill patients. At the conclusion of WWII, the Permanente Health Plan model was opened up to the public.
Today, Kaiser Permanente has grown remarkably and is one of the best-known systems in the USA. According to the Kaiser Permanente 2018 Annual Report, the health care plan has 12.2M members whose care is coordinated by 217K employees across 694 medical offices and other care facilities, 39 hospitals, 23K physicians and 59K nurses. Bernard Tyson, who has held the CEO position at Kaiser since 2013, reportedly was compensated $10M USD in 2016. In the first quarter of 2019, net “profit” for Kaiser Permanente was $3B USD. As a non-profit, Kaiser has $31.5B USD in reserves and 36 executives earning more than $1M USD a year. In short, the Kaiser model is a money-making machine.
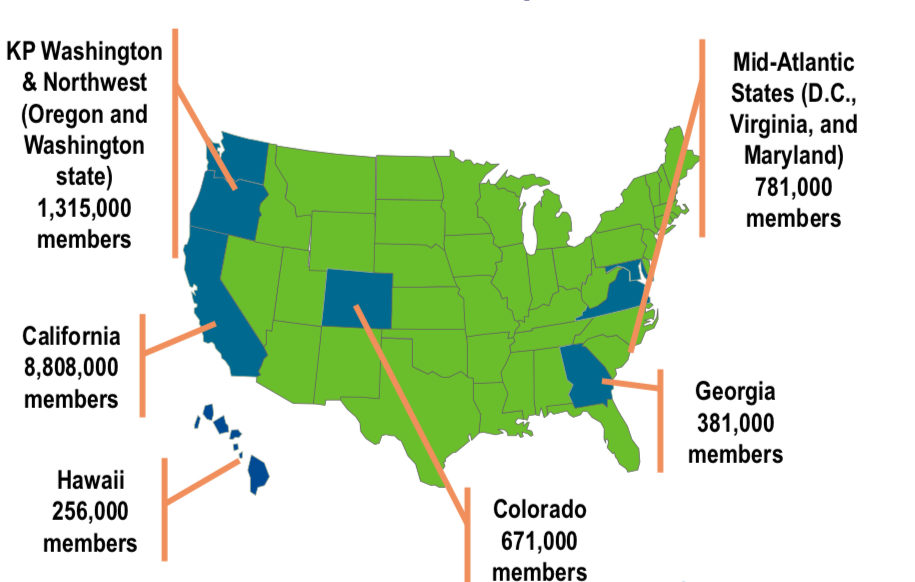
Kaiser Permanente Markets and Memberships (January 2018): Kaiser Permanente: Integration, Innovation, and Transformation in Health Care
With its steady flow of operating revenue, Kaiser Permanente provides comprehensive care to its plan members and invests heavily in information management technology (initially spending $6B USD on the KPHealthConnect Electronic Medical Record (EMR) with 6% of continuing revenues spent on IT) to enable seamless care and patient/provider access to data across the continuum of care.
Why then aren’t others adopting the Kaiser model of care across the United States and elsewhere? It offers a successful business model that delivers patient and provider satisfaction. Does it offer a fix for what ails high cost care in the United States and in other countries that are trying to rein in ballooning costs?
The Kaiser Permanente Model of Care
Kaiser Permanente care relies on the following entities:
- Kaiser Foundation Health Plan (KFHP): A non-profit health insurance plan which has a mutually exclusive contract with Permanente Medical Group physicians to provide care to their membership. The health plan offers benefits, enrolls members, and collects premiums.
- Kaiser Foundation Hospitals (KFH): A non-profit hospital system. The KFHP contracts with the hospitals to provide in-patient, diagnostics and ambulatory consultant care.
- Permanente Medical Groups (PMG): The medical groups are for-profit self-governed entities that have mutually exclusive contracts with KFHP for provision of health services to its members. Some Kaiser hospitals and medical groups contract with non-Kaiser Permanente physicians in order to service members. Kaiser physicians are paid a market-based salary for their services instead of fee-for-service compensation. Incentives for performance features such as access, patient satisfaction, and ensuring evidence-based care supplement physician salary as well as profit sharing through shareholder ownership of the PMG. The PMG receives a pre-determined payment from each Kaiser plan member every month through the KFHP whether or not the member receives services during that time period. This model of capitation is analogous to Family Health Organizations or other capitated primary care models in Ontario with a goal of providing high-quality, affordable care and managing population health rather than generating high volume of services. Unlike Ontario, the Kaiser capitated payment model extends beyond family practitioners to specialists.
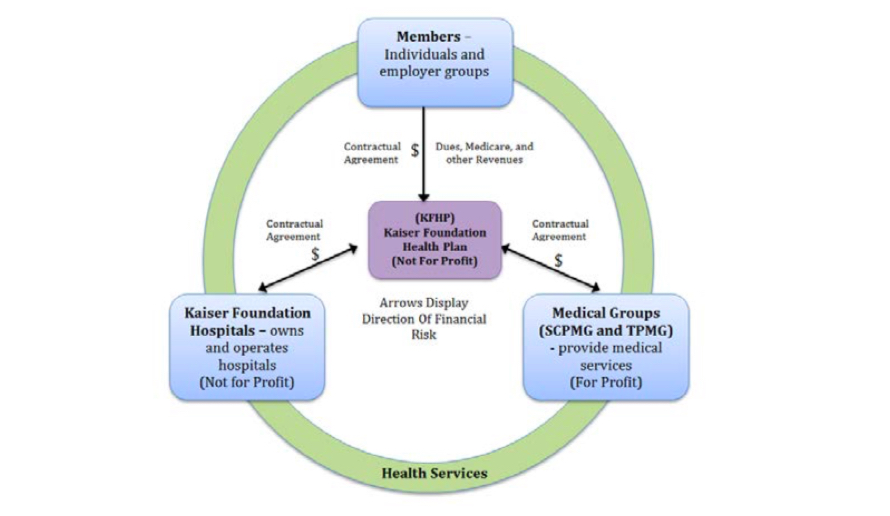 Contractual agreements between Plan members, Kaiser Foundation Hospitals, Kaiser Foundation Health Plan, and Permanente Medical Groups: Kaiser Permanente – California: A Model for Integrated Care for the Ill and Injured
Contractual agreements between Plan members, Kaiser Foundation Hospitals, Kaiser Foundation Health Plan, and Permanente Medical Groups: Kaiser Permanente – California: A Model for Integrated Care for the Ill and Injured
An important question that needs answering to understand the success of the Kaiser model is the composition and characteristics of the plan members. For example, are Kaiser’s patients mainly employed? Younger? Healthier? Do they enjoy higher socioeconomic status?
If so, a model of private voluntary insurance and user charges with the delivery of health care to a highly selected population would make it easier to keep patients out of hospital and control health care costs. The selective approach to coverage in the Kaiser plan is a major advantage over public systems like Ontario’s that need to cover all citizens regardless of health risks.
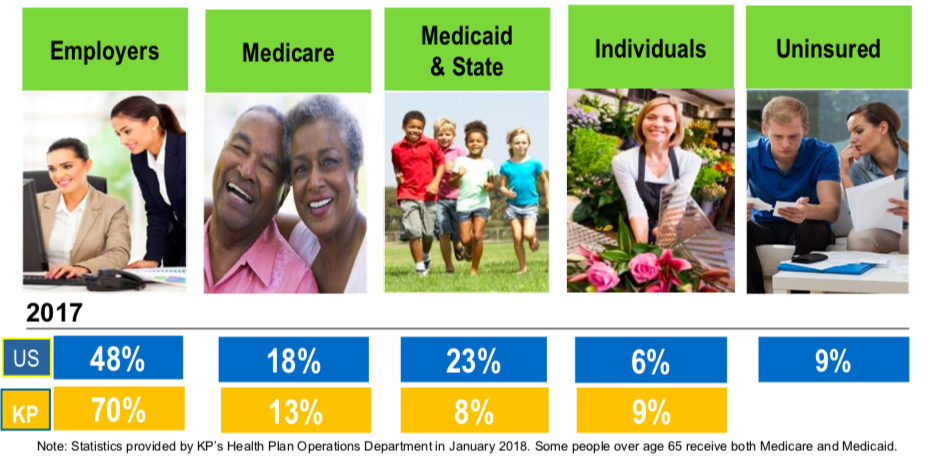
How Americans get their health coverage: Kaiser Permanente: Integration, Innovation, and Transformation in Health Care
The above graphic is from a March 2018 presentation slide deck entitled Kaiser Permanente: Integration, Innovation, and Transformation in Health Care, delivered by the Director of Kaiser Permanente International, Karin Cooke. This simple data set indicates that an overwhelming majority of Americans receiving health care coverage through Kaiser Permanente are employed (70%), compared to 48% of all Americans. The Kaiser population also includes relatively fewer older Americans eligible for Medicare than the general American population and has significantly fewer lower income people eligible for Medicaid.
As Michael Schull, CEO of the Institute for Clinical Evaluative Sciences rightfully points out in this article on the Healthy Debate website, this selective patient enrolment approach makes it difficult to use Kaiser as a model for a publicly funded, universal health system.
Others have criticized Kaiser for claims made in comparing Kaiser outcomes to international universal health systems. In 2002, an article in the BMJ (Getting more for their dollar: a comparison of the NHS with California’s Kaiser Permanente) suggested the Kaiser model performed better than the NHS. These claims were subsequently refuted by Talbot-Smith et al. in the British Journal of General Practice. The authors point out flaws in the Kaiser comparison data used to draw these conclusions — especially related to patient selection for the Kaiser insured population.
An important element to consider in evaluating the Kaiser model is their management of retirees and seniors. Few employers offer health benefits to their retired employees, and since 70% of the Kaiser covered population are insured through their employer, it is clear that relatively few retired Americans over 65 will rely on Kaiser as their health care costs escalate with aging.
It is also apparent that Kaiser insurance becomes supplemented by Medicare Parts A and B as the insured client reaches 65. Clients working beyond 65 may continue their Kaiser plan supplemented by Medicare insurance. So, workers continuing employment insurance beyond 65 supplement Kaiser coverage with Medicare. As they retire, most people will find themselves no longer insured by Kaiser and will rely only on Medicare if their employer does not offer retiree insurance through Kaiser.
Can the Kaiser Permanente model work in Ontario?
The Ontario health system is about to undergo substantive change, with the first round of successful Ontario Health Team (OHT) candidates to be announced in the summer or fall of 2019. In the resources for health care providers that the Ministry provided on their website to assist in the OHT application process, Kaiser Permanente was a suggested integrated system in the jurisdictional scan of eight integrated care systems. Interestingly enough, in their presentation on Kaiser Permanente, the Ministry stated that no information was provided on Kaiser financial performance measures.
So, what should we learn from Kaiser Permanente and its adaptability to the Ontario healthcare system? Matthew Townsend provides an excellent review in Learning from Kaiser Permanente: Integrated systems and healthcare improvement in Canada prepared for the Canadian Foundation for Healthcare Improvement in November 2014.
Here are some key points to consider:
- According to the Fiscal Accountability Office, the Ministry of Health and Long-Term Care (MOHLTC) has 2019 operating revenues of $61.3B CDN or $45.77 USD that serves a population of about 14M citizens. Kaiser Permanente has an operating revenue of $79.7B USD that serves a population of 12.2M. A comparison of per capita cost shows that the Kaiser model ($6533 USD) is considerably more expensive than Ontario’s system ($3264 USD).
- With this operating revenue, the MOHLTC administers approximately 160 general, rehabilitation, continuing care and specialty psychiatric hospitals while Kaiser Permanente administers 39 Foundation hospitals.
- Kaiser Permanente employs 23K physicians who are paid a salary rather than fee-for-service. The MOHLTC pays about 31K physicians who are compensated on both fee-for-service and capitation-based models.
- Both the MOHLTC and Kaiser Permanente provide a suite of comprehensive inpatient/outpatient services. However, there are copayments on many of the services provided by Kaiser Permanente that must be paid in addition to their monthly premium.
- Comparing ambulatory care coverage, dental and drug coverage is generally provided under many of the Kaiser Permanente care plans and not widely covered under OHIP. On the other hand, long-term care and complex continuing care coverage is not paid in the Kaiser Permanente model. The MOHLTC currently spends more than $4B annually on long-term care and is investing heavily in opening of 10,000 new long-term care beds to manage increasing numbers of frail seniors in Ontario.
- Administratively, Kaiser Permanente spends much more on bureaucrats to operate their health care plan than the MOHLTC. Much has been made of Ontario health care’s so-called ‘bloated bureaucracy’ when critics dissect problems in our system. What would these critics say about a CEO who gets compensated $10M USD annually and 36 executives earning more than $1M USD a year?
Can Ontario Health Teams learn important lessons from the Kaiser model? Absolutely.
There is no question that we need better integrated care in Ontario. The Kaiser model has achieved integration with its entire care team through seamless communication using integrated information technology. Kaiser Permanente’s HealthConnect was successfully rolled out between 2004-2010 and is much more comprehensive and user friendly than anything Ontario currently has on offer. Can Ontario achieve the same integration through interfacing of currently available IT resources? Will it need to offer all OHTs access to a new system similar to KP HealthConnect?
The Kaiser culture also stresses a consistent measurement and comparison of outcomes aligned with proper structure and incentives to encourage evidence-based care – a key component of a learning healthcare system. Remembering that physicians in Ontario are more independent contractors than in the Kaiser system, will professionals in Ontario allow management structures that enhance quality improvement within their practices and compensation models?
What about buy-in for the Kaiser capitation-based model for Ontario’s doctors? It is unlikely that doctors in Ontario would readily agree to a Kaiser model of capitation without substantial increases in pay and benefits possibly including pension benefits. It is not clear whether physicians would generally accept a Kaiser compensation model as part of the OHT transformation and very unlikely that the province could afford the model.
The Kaiser model of care is for doctors who feel comfortable with its vision. It is clear that the Kaiser compensation model is not acceptable to all American physicians and those who don’t concur with the Kaiser model leave. In Ontario, there is no alternative employment model available for physicians. Retaining autonomy is an important issue for Ontario physicians and will likely be an important factor in achieving success with the Ontario Health Teams.
As our healthcare system in Ontario continually evolves, we need sound evidence to guide decision making. Like the Golden State Warriors, Kaiser Permanente is often referenced as the gold standard, a benchmark that defines excellence.
While that may be true for the NBA’s current dynasty, the Kaiser Permanente model of care is built on a framework that would exclude many Ontarians from receiving treatment for medically necessary services. The Kaiser model would also cost Ontarian tax payers substantially more than our current system for providing less insured service. Insuring lower risk individuals at higher cost for less insured service is a good recipe for making money but is not practical for a universal, taxpayer-funded system.